Research and develop innovative and leading edge information systems in healthcare, with applications in emergency medical care and public health surveillance and distance education.
The highly centralized and hierarchical approaches for large-scale dissemination of health care services (HCS) provision, commonly found in global initiatives for health care, is not suitable for the for the dynamic and unpredictable ways in which such services can expand and be sustained. In the same way, the infrastructure of the Information and Communication Technologies (ICTs) to support the HCS in these approaches also faces difficulties in handling such change and unpredictability in a sustainable fashion. In general, to emphasize detailed initial planning and projects with low flexibility, which in the long term tend not to be successful, the example of projects that create islands of excellence, but which are not sustainable when their sources of funding cease. The realization of these difficulties in recent years has spurred the design of a new paradigm, based on the vision of providing health care services as socio-technical systems with characteristics of complex adaptive systems.
The phrase complex adaptive socio-technical systems, in the context of providing SAS(HCS), refers to the interaction between people, technology and the environment in which they are placed, comprising a large number of components, such as patients, healthcare professionals, service providers, health plans, equipment, administrators and of health care policy designers. The complexity of the interaction between these components generates structures and behaviors which are difficult to predict and understand, and which evolve to a level of organization-based self-adaptation instead of centralized control. For existing or new problems in providing SAS, there are always health professionals with an interest in devoting time and effort to resolve them as a natural part of their professional interests, with or without adequate funds available. With professionals being naturally organized in scale free networks, those most influential (hubs) can be spontaneously encouraged to collaborate with others to resolve a particular problem, influencing attitudes and practices pervasively, starting from the closest and reaching gradually to the most distant and weakly connected, with effects not planned beforehand. Examples of such self-propagation networks can be found in the work of Joanna Briggs, Institute for Health Care Based on Evidence (www.joannabriggs.edu.au).
It is important to note that the research and development activities presented in Sections 5.1.1 to 5.1.8 allow the development of different systems of high computational complexity potentially acting independently in different areas of health. Some of these systems are described in more detail in Section 5.1.10. However, it can be clearly seen that any combination of these systems take the form of a complex adaptive socio-technical system. The challenge is how to induce the movement of building an infrastructure for such systems that is sustainable, considering that traditional methods of software and systems engineering employ development approaches that do not correspond with its complexity, like the absence of central authority and design without a specifications.
Considering the current organization of public health services in Brazil in three levels of care - primary, secondary and tertiary - we can classify the types of systems originating from other areas of the INCT- MACC as related to secondary and tertiary care, i.e., to procedures of medium and high complexity. In this scenario, the collection of data related to population health - essential for proper validation, calibration and operation of these systems - plays a critical role. In the national context, the Family Health Program (PSF FHP), designed to bring health care closer to the population, offers the means for collecting these data. The PSF is performed through regular home visits with the help of Family Health Teams (FHT). The data collected during these visits are collected using standardized forms, digitalized in a standard SUS information system. After anonymization, these data are made freely available by DATASUS (the Informatics Department of the Unified Health system –SUS-). The information provided by this infrastructure can then be used by healthcare managers to plan their actions to promote healthcare. One of the biggest problems with methods of data collection based on paper is the low quality of the data generated, as well as the huge delay for data to be made available due to the elapsed time between its collection and digitization. However, even if online electronic health records (EHRs) were employed, the complexity of health information makes the development of these records a challenging activity. Firstly, the dynamic nature of health systems and biomedical science in general, makes it difficult to maintain the systems, since maintenance has to be accomplished with a much higher frequency than in other sectors of the economy, which increases the price of the final product. Moreover, the huge number of concepts in biomedical sciences (somewhere around 300,000 terms) and the difficulty of reaching consensus among experts about the representation of the result of medical knowledge generates an extreme variability of the system requirements, even within the same level of complexity of care. Finally, the route of the patients through various health services, and the fact that the results of a consultation can affect the outcome of the subsequent consultations, make the acquisition of semantic interoperability a basic need for the field of health informatics. Information and knowledge are the raw materials for performing all actions to control and prevent diseases. Currently the health information systems produce huge amounts of data, which may be located locally in a given institution or centralized and available in the IT systems of the SUS. The great challenge is to identify and implement appropriate methods and tools capable of transforming this huge dataset into information and knowledge useful for healthcare promotion.
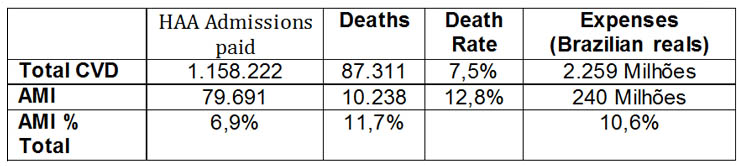
Another important issue related to the levels of primary and secondary care is the difficulty in proper emergency care for complex cases such as those related to cardiovascular disease. Cardiovascular diseases are the leading cause of morbidity, disability and death worldwide and in Brazil. Most deaths from heart attacks occur in the early hours of onset of the disease - 65% of deaths occur in the first hour and 80% within 24 hours after the onset of infarction. The following table summarizes information about Acute Myocardial Infarction (AMI) with respect to Cardiovascular Diseases (CVDs) from January to December 2011, according to DATASUS.
Approximately half of the patients who suffer an AMI will be recommended the use of thrombolytics or primary angioplasty. However, it is estimated that only 10 to 15% receive such treatment. Therefore, despite the reimbursement of thrombolytic therapy by the SUS, between 85 and 90% of patients with myocardial infarction remain only on observation and treatment of complications.
Among the main difficulties for adequate healthcare are: 1) Interest and training of professionals; 2) Existence of protocol and qualification for application; 3) Availability of performing an ECG within 10 minutes; 4) Correct identification of ischemic ECG vs. nonischemic; 5) Availability of troponin and CK-MB; 6) Overcrowding of health facilities.
The delay in proper treatment of cardiovascular diseases makes the process more expensive. An example is provided by the expenses with congestive heart failure (CHF). CHF is the syndrome that follows in the majority of cases of heart disease, one of the sequelae of myocardial infarction not treated appropriately. It is the third largest cause of hospitalization in Brazil, consuming 2.6% in 2011, and 3.6% in years before 2011, of all resources invested in health by SUS. In 2011 what was spent on hospitalization for CHF accounted for 27% (R $ 305 million) more than all that was spent on AMI.
Within this context, there is a large number of doctors, acting in the levels of primary and secondary care in the SUS, who make contact by telephone with the Emergency Unit of the Heart Institute, to ask questions about their medical cases and who do not have anyone else to discuss the matter with. It is assumed that this contact will be made only by a very small percentage of physicians who have doubts, as this service is a consultation of entirely informal nature, and the receipt of this information depends on the availability and willingness of hospital staff. But still this fraction gives an idea as to the magnitude of the lack of information and the possibility of debating and resolve doubts in emergency cases that exist in Brazil, and serves as a warning for the development of solutions to this problem.
The development of methods to improve the treatment of a cardiovascular emergency at the time of its occurrence can mean reduced sequels for the patient and, in addition, generate substantial savings to the health system. Currently, telemedicine and telehealth are instruments that offer an ample amount of resources for education, care and research at a distance. It also allows the creation of tools and solutions that can be used at the state or national level.
In addition to emergency care systems, clinical decision support systems (CDSS) are other examples of complex systems that handle different types of medical information. CDSS are expert systems that provide information, alerts and recommendations to physicians, based on clinical observations of the patient, aimed at assisting decision making at the time of clinical care. A CDSS can provide as output, for example: clinical diagnosis, most likely based on clinical manifestations presented by the patient, care treatment plans, follow-up treatment of the patient based on medical protocols and generation of alerts and reminders, activated by a rule-based system implemented in a knowledge base.
The use of CDSS can help the physician in the selection of information and evaluation of the patient’s clinical context or can help with clinical care when experts are not available for the disease of interest. There is evidence to indicate that the use of CDSS in clinical practice improves the quality and efficiency of the diagnosis, provides greater safety for patients and reduces costs associated with the health care system. For a CDSS applied to diagnosis, two areas are involved during its modeling and development: the domain of clinical information and the knowledge base. It is essential to adopt a data model to ensure structural and semantic interoperability of clinical information model with the diagnostic criteria mapped in the knowledge base. Mapping the knowledge base by the domain expert (doctor) can be facilitated with the use of ontologies and a knowledge acquisition tool.
Some factors influencing the use of CDSS are friendly computer interfaces, the management of large amounts of information for medical diagnosis, recognition of the potential of using computational tools to improve clinical practice and pressure from administrative institutions and government to adopt more effective practices and evidence-based medicine. Some benefits are the support of administrative functions, management of clinical complexity, cost control, clinical diagnostic support and therapeutic procedures using best practice, and population management for epidemiologic study.
Activities
- Develop tools for clinical case discussion and health information sharing in a collaborative environment, ensuring confidentiality and data security. The use of computational tools for the discussion of clinical cases allows, in theory, for integration between existing hospital information systems and systems for case discussion. This link is quite interesting, as it allows knowledge, which is usually accessible only to a small group of professionals, to be shared with other professionals.
- Develop a toolkit for primary care, able to offer mobility solutions for collecting and georeferencing health information at the point of care or at the residence of the patient / user of the public health system.
- Develop a set of methods and tools to extract information and knowledge from large health databases.
- Investigate and develop targeted approaches to multilevel models of data, including openEHR (http://www.openehr.org) and MLHIM (http://www.mlhim.org), as a way to promote semantic interoperability between health information systems.
- Study and develop computer decision models applied to clinical diagnosis. The decision model should include partial observations and treatment of uncertainty, features present in the clinical context, and also a qualitatively modeled knowledge base, based on the medical literature, and quantitatively using clinical cases of patients and normal controls. The decision model should be represented in a legible to the doctor or the domain expert graphic language, and systems analysts.
- Study and develop models for an information infrastructure capable of operating as an adaptive complex socio-technical system, characteristic of the systems previewed in this project. The design of such a model should seek a reconciliation of tensions between the demands from local and global health care services as well as the tensions present in the socio-technical process of building the infrastructure, and tensions arising from the demands of the individual and community.
- Development and implementation of CDSS using the proposed computational model for decision support in the routine care of a health facility. The implementation should include usability testing with application users, who will be doctors, nurses or people responsible for patient care in this health unit.
- Refinement of the decision model and extension to other care units and healthcare institutions, such as imaging clinics, clinical analysis laboratories and outpatient care points. The aim is to validate the generality of the decision model in other activities of routine clinical practice and disease domains, based on methods and evaluation strategies. Thus, in addition to predisposing factors, symptomatic information, and signs of the disease, results of imaging studies and laboratory tests can be integrated as an input to the decision model.
- Development, implantation and evaluation of a ubiquous computational system to monitor, collect and process physiological data of people performing physical activities together with the unified public databases. This system must operate indoor (arenas, stadiums, recreation places) as well as outdoor (parks, public places, etc.).
- Development, implantation and evaluation of a computational system for the academic and pedagogic management of courses in the area of Health that deal with active teaching/learning methodologies. Particularly, the system must have a reflexive electronic record to evaluate students and professor performance in these courses.
Goals
- By the end of 2017: to have a mobile system for the collection and georeferencing of primary care information.
- By the end of 2017: to have an application for the extraction of health information from a healthcare record database.
- By the end of 2019: to produce multilevel models for the Death Information System (DIS) and Hospital Information System SUS (HIS-SUS), and for the detailed clinical models Common Data Elements (CDE) and United States Healthcare Information Knowledgebase (USHIK).
- By the end of 2021: to produce an analysis of performance indicators for multilevel models with respect to implementations of SIM and SIH-SUS systems and of the detailed clinical models CDE USHIK.
- By the end of 2017: to develop a model for decision support to clinical diagnosis and a representation model for the diagnostic procedures for diseases associated with aging and / or diseases of the breast, integrated into a CDSS.
- By the end of 2019: Deploy the CDSS in a clinical setting and evaluate the developed system.
- By the end of 2021: Extend the CDSS to other diseases and / or institutions, evaluating the results generated in the health system.
- By the end of 2021: Develop, implement and evaluate a monitoring system that collects and processes physiological data of people involved in physical activity.
- By the end of 2021: Develop, implement and evaluate a management system of academic and pedagogic activities for courses in the health area that employ active teaching/learning methodologies.
Impact
Developments in this area will ensure:
- Availability of primary care data for health managers in real time and with higher quality.
- Availability of specialist opinion in cardiological emergency for interaction in real time, providing (i) agility in diagnosis and identification of cases in need of urgent referrals, and reduction of unnecessary referrals, (ii) agility and efficiency in decision making which may reduce morbidity / mortality, (iii) greater security in patient intervention and the possibility (JAS: ?) and clinical follow-up of the patient at a distance; (iv) systematic standardization of Telepropedeutic in emergency, and training of all professionals involved; (v) storage of clinical data for epidemiological surveys; (vi) creation of databases for registration and the subsequent registration of resources available in each center of the collaborative network; (vii) creating short course for training of professionals in the areas of emergency and urgency; (viii) training of interactive educational components (units of knowledge) to facilitate the standardization of practices and procedures.
- Extraction of information and knowledge that will enable more effective action in public health.
- Building a better system of government for citizens, and enhancing the participation of citizens and groups in political processes and decisions, since information collected by systems based on multilevel models allows DATASUS information systems to be informed with more timely and better quality data.
- Decision support systems can improve the quality of medical diagnosis, improve patient safety and reduce operating costs of the health system. They may also allow a better understanding of disease etiology by mapping the diagnostic criteria for a knowledge base.
- Improvement in the formal health education system

